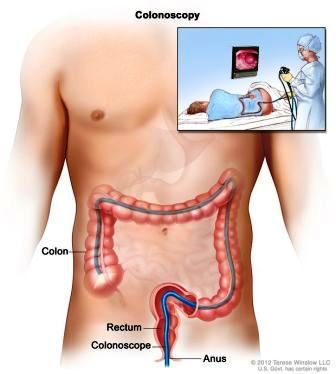
What is a colonoscopy?
This is a short procedure to examine the lining of the lower part of the digestive tract. Under sedation, a thin flexible tube camera is passed into the rectum and gently moved along the colon (inflating then deflating with air) to where it meets the small intestine. A magnified image of the colon’s inner surface is projected on a TV screen. The test takes about 20 minutes. Plan 2 – 4 hours for waiting, preparation and recovery and bring a good book.
Who is responsible?
Dr Douglas Samuel will perform the test. An experienced team lead by an anaesthetist will sedate you and ensure your comfort and safety.

What happens before the test?
On booking, you will be given an endoscopy session (eg. Monday afternoon 5 September 1-6pm). Occasionally, we may call you to change it. To change or cancel your booking, please call my rooms as soon as possible, to allow for others on the waiting list. You will be scheduled at one of the below endoscopy units:
1. North Shore Private Hospital (NSPH)
Please complete online admission form at least 3 working days prior to your test. If you prefer paper admission forms (available from our rooms), please deliver papers to NSPH reception or the NSPH bookings department (fax: 8425-4121; mail or email: nspbook@ramsayhealth.com.au). NSPH staff will call to confirm your admission time on the afternoon 3-6pm before your test (or Friday for a Monday test). Please contact NSPH billing department for any hospital billing inquires (tel: 84253000). Dr Samuel or our practice nurse Sr Jenny Burns RN will contact you a few days before and after your procedure to help you prepare for the day and provide you with extra support. The NSPH Day Surgery unit is located in the Health Hub building, entry is via Reserve Road or Westbourne Street, take the Tower A lifts to the podium level and follow the signs to Day Surgery (click here for: Patient Journey Video).
2. North Shore Specialist Day Hospital (www.nssdh.com.au)
Please complete the online admission form below (preferred method). If you would prefer to complete a paper admission form (download here or available from our rooms), please return at least 7 days before your procedure to NSSDH admissions coordinator, Kim (tel: 9425 1678; fax: 80886777; email: admin@nssdh.com.au). NSSDH staff will call to confirm your admission time on the afternoon (2-5pm) before your test (or Friday for a Monday test). Our practice nurse sister Jenny Burns RN will call you a few days before your procedure to help prepare you for the day.
3. Mayo (MPH) and Forster Private Hospital (FPH)
Please complete the online Pre-Admission Form here. This form should take you approximately 30 minutes to complete. If you have any problems completing the form or would like fill out the paper version, please contact: the MPH admissions coordinator via: mayo.admissionforms@healthecare.com.au or 65393600 option 1; or for Forster Private Hospital the FPH day surgery coordinator via: ftr.admissions@healthecare.com.au or 65551555. Our practice nurses sister Donna Chant RN (MPH) or Katrina Hansen RN (FPH) will call or see you a few days before your procedure to help prepare you for the day. You will be contacted with your admission time the day (FPH by 11am, MPH by 4pm) before your test (or Friday for a Monday test).
Can I take my current medications?
Most medications (including aspirin) can be continued. Be sure to tell our staff if you have:
1) drug reactions or allergies,
2) need for antibiotics for dental procedures and,
3) taken in the past 3 months: "the pill", aspirin, blood thinners (eg. warfarin, clopidogrel, rivaroxaban), insulin or prednisone.
If you are on the “pill,” use another contraceptive for 2 weeks after your procedure. Stop anti-diarrhoea or iron pills five days before. Aspirin can be taken as usual but other blood thinners will need special instructions. If you use steroid puffers as asthma preventers, use them at usual or increased dose for 5 days before the procedure to ensure your lungs are at their best. If you have diabetes and take diabetes pills or insulin - then on test day, these must not be taken unless instructed AND on the day before the test, take half the usual insulin and be careful with “hypos”. Bring an up-to-date list of all your medicines to hospital.
What about COVID?
In most case, you can proceed with bowel preparation and the procedure if:
- RAT test is negative
- You had a mild COVID illness and are more than 4 weeks from first diagnosis
- You were admitted to ICU with severe COVID and are more than 8 weeks from first diagnosis
- You don't have a reasonable suspicion that you are infectious with COVID
- You are a close contact and COVID negative x 2 (on bowel prep and test day)
- You have mild respiratory symptoms and are COVID PCR negative within 3 days of the test and RAT negative on test day
What are the risks?
Before your procedure, you will have an opportunity to ask questions particularly about the benefits and risks of your colonoscopy and have these answered in a way that you understand. Colonoscopy is very safe. After bowel cleansing laxatives, nausea and bloating is common and rarely lasts long. Unusual colon anatomy or poor bowel cleansing sometimes make completed colonoscopy impossible. In this case, your doctor may order a redo colonoscopy on another day or, another test or, he may feel the limited examination is enough. To maximise your chance of a good bowel preparation, follow the bowel cleansing instruction below (which include taking laxatives 4-5 hours before afternoon procedures (ie. don't follow the instruction in the Prepkit C packet). Even with the best techniques, polyps and tumours can be hidden from view and missed.
The bowel wall may be unusually fragile and puncture or bleed. Bleeding after polyp removal is usually minor and stops on its own. Complications needing urgent surgery are rare (1 in 1000). Other uncommon problems include sedative or bowel preparation reactions, infections or worsening of existing heart or lung disease. Occasionally you may wake with a sore angle of the jaw after the anaesthetist has pushed firmly here to keep you safe during your test. This tenderness usually settles after a few days. Aspiration- related chest infections while sedated are uncommon with an empty stomach particularly if you fast as instructed. Although complications are uncommon, it is important to recognise them early. Contact your doctor or hospital if you notice severe abdominal pain, dizziness, fever, chills, rectal bleeding (more than 1/2 a cup) or severe shortness of breath.
Your risk of major bleeding after polyp removal continues up to 10-14 days with the greatest risk within 48 hours. Air travel is not safe for domestic flights within 2 days and; long haul flights and travel to remote areas within 5 days if you have had a polyp removed.
Are there alternatives?
Colonoscopy is considered the best test for same time diagnosis and treatment for bowel cancer prevention and detection of polyps. CT scan and stool testing may have a role. Discuss the alternatives with your doctor to help choose.
Bowel cleansing: in 3 steps
This is usually the most troublesome part of your procedure:
48-24 hours before colonoscopy
"THE WHITE DIET" with LOW ROUGHAGE/FIBRE
No seeds including bread with seeds, nuts, uncooked vegetables, skins and whole grains
Enjoy "the white diet": white rice/bread/pasta, rice bubbles or cornflakes, congee, fresh white fish, poultry (without skin), bacon, pork or chicken sausage, eggs (one yolk only - eg, white scrabbled eggs with 1 yolk), boiled peeled potatoes or pumpkin, potato salad (without skin or greens), hash browns, canned or well cooked vegetables without skins or seeds. Milk and foods made from milk if tolerated eg. plain yoghurt, margarine, butter, ice cream, chocolate, cream/cottage/ricotta/fetta cheese. Macaroni cheese or pasta carbonara (no tomato or bottled sauces), plain bagels or white toast with vegemite/honey/lemon butter/butter, French or cinnamon toast, plain or ham/cheese croissant, honey and crumpets or pancakes, chocolate brioche, rice custard, chocolate mouse. cheese and crackers/rice cakes, protein bars without nuts or seeds, wedges with sour cream, ham quiche, parmesan cheese sticks, scones with honey, waffles or pikelets with lemon/sugar/honey.
Enjoy all clear fluids below. If you prefer raw fruits and vegetables, use a juicing machine to remove their pulp before consumption.
Avoid these white foods: pears, parsnip, cauliflower, onion, high fibre white breads (e.g. Wonder White), tofu, coconut, porridge, banana, mushrooms, semolina, couscous, popcorn
24 - 2 hours before colonoscopy
CLEAR FLUIDS ONLY (NO SOLID FOOD)
Water, clear fruit juices (apple, pear, white grape), coconut water, jelly, skim milk, Bonox, black tea/coffee, honey, carbonated beverages, clear cordials (lemon/lime), Ensure ® (<3 cans), sports drinks (eg.Gatorade ®), popsicles, sorbet/gelati. Clear broth/bouillon or Vietnamese pho broth (STRAIN chicken/ beef/vegetable noodle soups), thin congee, Hard/gelatine sweets (eg. barley sugars, lollipops, gummy bears), small volume of clear alcohol (light beer, white wine, vodka, gin, whiskey etc)
No solid food, full cream milk; no red/purple food colouring for 24 hours

Take care to avoid dehydration.
Drink 2-3 glasses or serves of clear fluids throughout the day at: breakfast, morning tea, lunch, afternoon tea, dinner and evening (and test morning up to two hours prior)
IT’S CLEAR, IF YOU CAN READ NEWSPAPER THROUGH IT

Buy Prepkit Orange or Prepkit C (3 sachets) well in advance from a local pharmacy
(No prescription required):
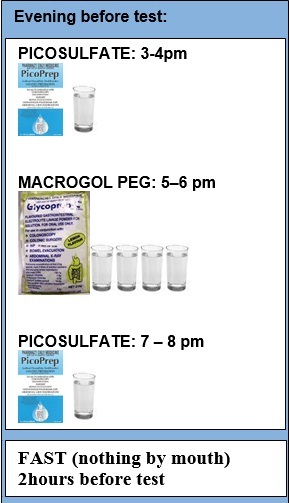
"PICOPREP" (x2 picosulfate): add (sachet A or C) to ONE 250mL glass of warm water (if preferred, chill in a refrigerator before drinking), drink over 30 minutes
"GLYCOPREP C" (x1 macrogol): add (sachet B) to FOUR 250mL glasses (or 1L jug) of warm water (if preferred, chill in a refrigerator before drinking). Drink 1 glass every 15 mins. If you start to feel nauseous, slow down
take two sachets the evening before and one on test day
Expect diarrhoea (30 mins to 4 hours) after drinking laxative sachet
FOR COLONOSCOPY AFTER 10AM*
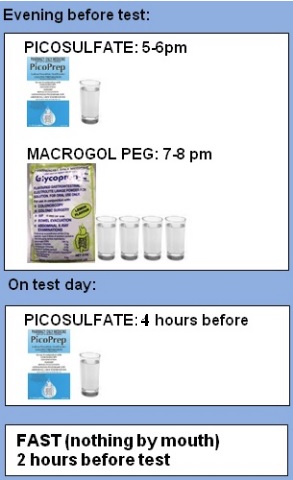
FOR COLONOSCOPY BEFORE 10AM*
* FOR COLONOSCOPY BEFORE 10AM
Your options for the third (Picoprep) sachet depend on when you like to sleep. They are to take it:
- at 9pm (ie take each at 5pm, 7pm, 9pm) - most common
- at 3pm (ie take each at 3pm, 5pm, 7pm)
- 4 hours before (eg. for a 10am test, after setting your alarm! take each at 5pm, 7pm and the next day at 5-6am )
TEN TIPS FOR SURVIVING BOWEL PREP for YOUR COLON PHOTO SHOOT
- Prepare laxative mixtures in advance and chill well
- If you feel nauseous, slowing down is usually enough. If severe nausea or vomiting is your concern, ask your doctor for ondansetron (Zofran) an hour before the first laxative dose and every six to eight hours during the process. This is effective for most people.
- Add lemon juice, ginger ale or lime cordial (but only if you never want to drink that beverage again in your life ! )
- Chill glass, drink with a straw and rinse mouth after drinking
- Suck on sweets
- Stock up on peppermint tea, lemonade iceblocks and ginger ale beforehand
- Apply Vaseline or Zinc oxide to your anal area in advance and use baby wipes instead of toilet paper
- Ensure safe, well-lit bathroom access, particularly at night, to prevent falls or accidents
- Don't be afraid to bring some entertainment to the bathroom, you'll be there a while
- Drink clear fluids right up to 2 hours before your test
If you feel you'd be more comfortable to be admitted the night before your colonoscopy for extra nursing care, please let our rooms know.
Sister Jenny Burns RN, our North Shore endoscopy practice nurse, will give you her number when she calls before and after your procedure. Sr Jenny is available to you if you would like to speak with her about your procedure or bowel preparation or you may like to call the hospital to speak with our endoscopy nurses.
SPECIAL GROUPS
These conditions may need a little extra attention and special instructions for bowel preparation:
- colonoscopy before 10am (see above)
- augmented/extra prep:
- diabetes
- severe constipation
- prior inadequate bowel preparation
- Moviprep only for:
- severe kidney disease (eGFR<30)
- liver cirrhosis (on spironolactone)
- heart failure (on frusemide/spironolactone or EF<40%)
- Avoiding liquid prep
- impaired swallow on grade 1-2 thickened feeds grade 1-2
- capsule based or anti-nausea meds for liquid prep intolerance
Special groups
These conditions may need a little extra attention and special instructions for bowel preparation:
- colonoscopy before 10am (see above)
- augmented/extra prep:
- diabetes
- severe constipation
- prior inadequate bowel preparation
- Moviprep only for:
- severe kidney disease (eGFR<30)
- liver cirrhosis (on spironolactone)
- heart failure (on frusemide/spironolactone or EF<40%)
- Avoiding liquid prep
- impaired swallow on grade 1-2 thickened feeds grade 1-2
- capsule based or anti-nausea meds for liquid prep intolerance
What if something abnormal is found?
If an area needs further testing, you will have a biopsy (a rice grain-sized sample of colon lining). Bleeding problems may be controlled with special techniques. Usually, if you have polyps (benign growths on the colon lining) these will be removed called polypectomy. Polypectomy is an important way to prevent bowel cancer. Biopsy and polyp removal is not painful. If haemorrhoid bleeding or discomfort are a significant problem, ask about treating these while sedated with non-surgical techniques including rubber band ligation or infrared coagulation. These haemorrhoid treatments, while associated with less pain and risks than haemorrhoid surgery, may cause manageable short term pain or discomfort for a few hours to days.
What happens after colonoscopy?
On waking, you may feel wind pain, bloating and pass air introduced during the test. You may have discomfort at the vein access site on your arm. Even if you feel alert, your judgement, memory and reflexes will be impaired for the rest of the day. Your doctor will see you after the test and give you your results with a written report. It is common to have no memory of the test or discussion. Someone familiar must drive you home and stay with you after the procedure. Our hospital policy does not allow taxi services. Do not drive your car, sign legal papers or send important emails, drink alcohol or operate machinery until the next day. A report with biopsy results will be sent to your referring doctor after about a week. It is important that you ring the rooms to make and keep a follow up appointment with your specialist to discuss the results.