Small and large intestine

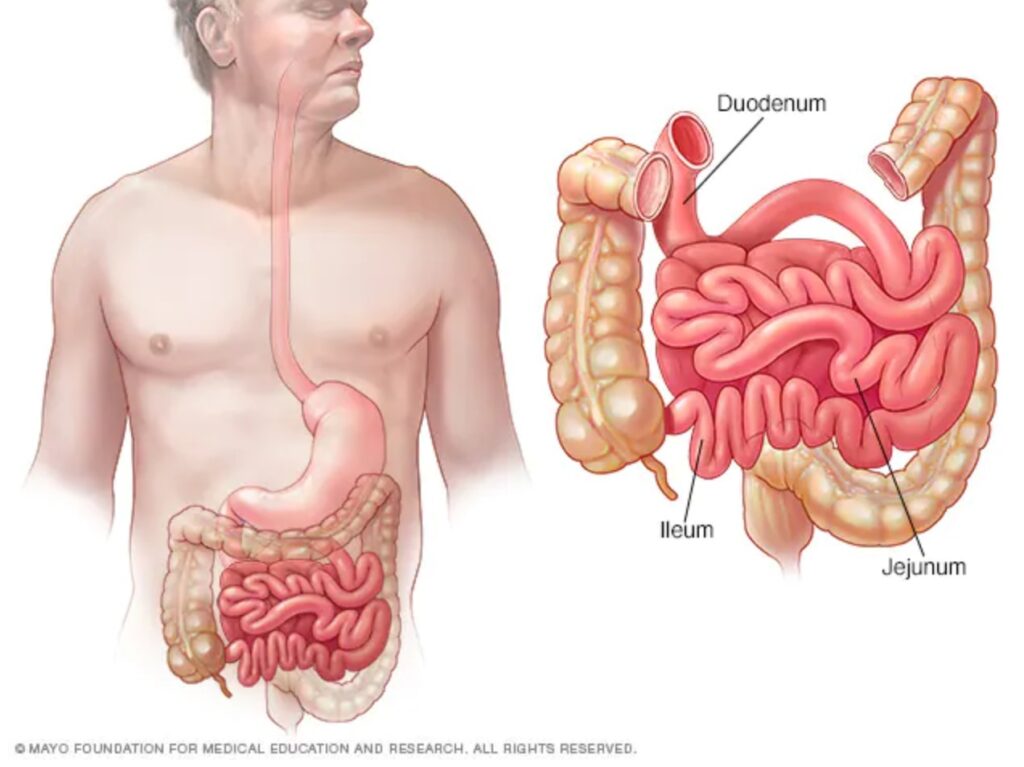
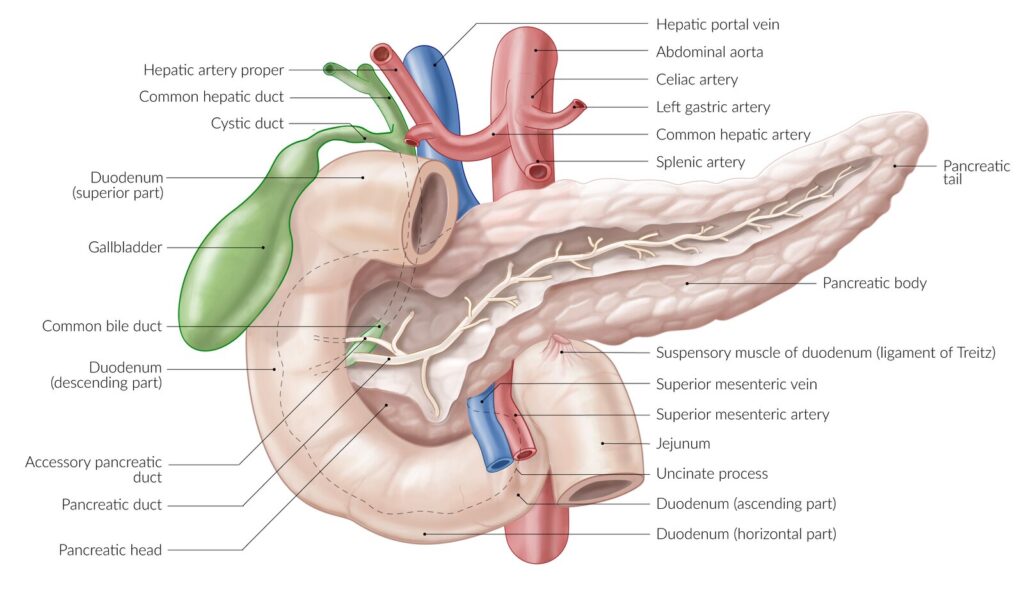
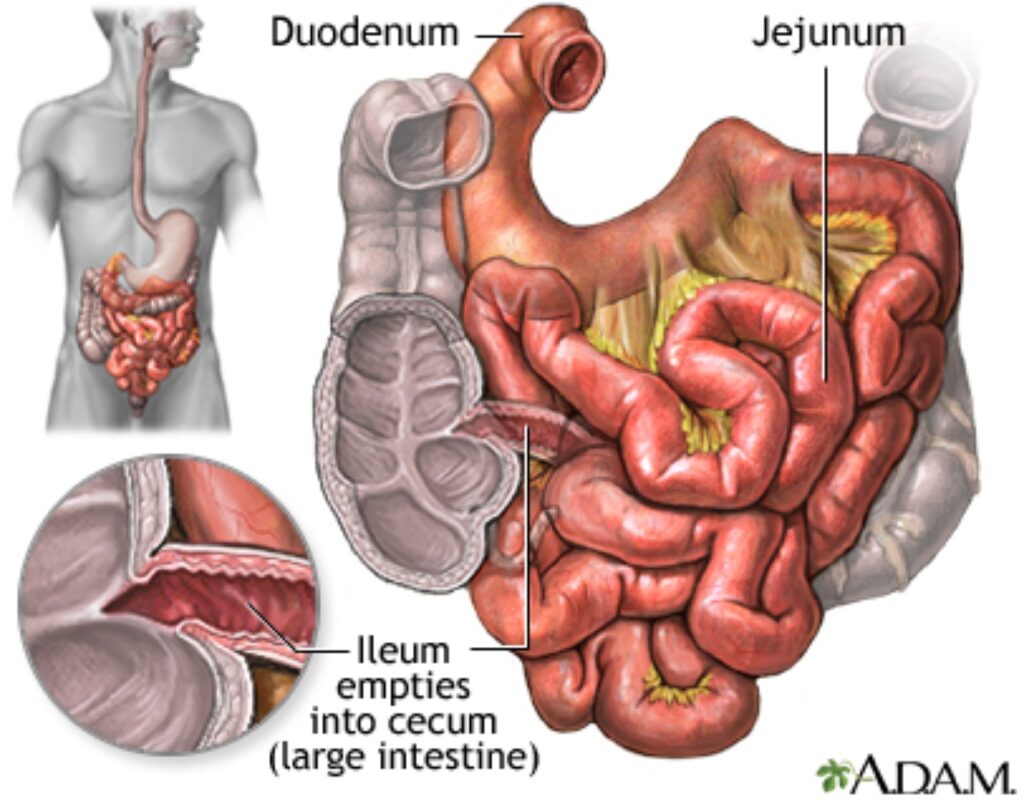
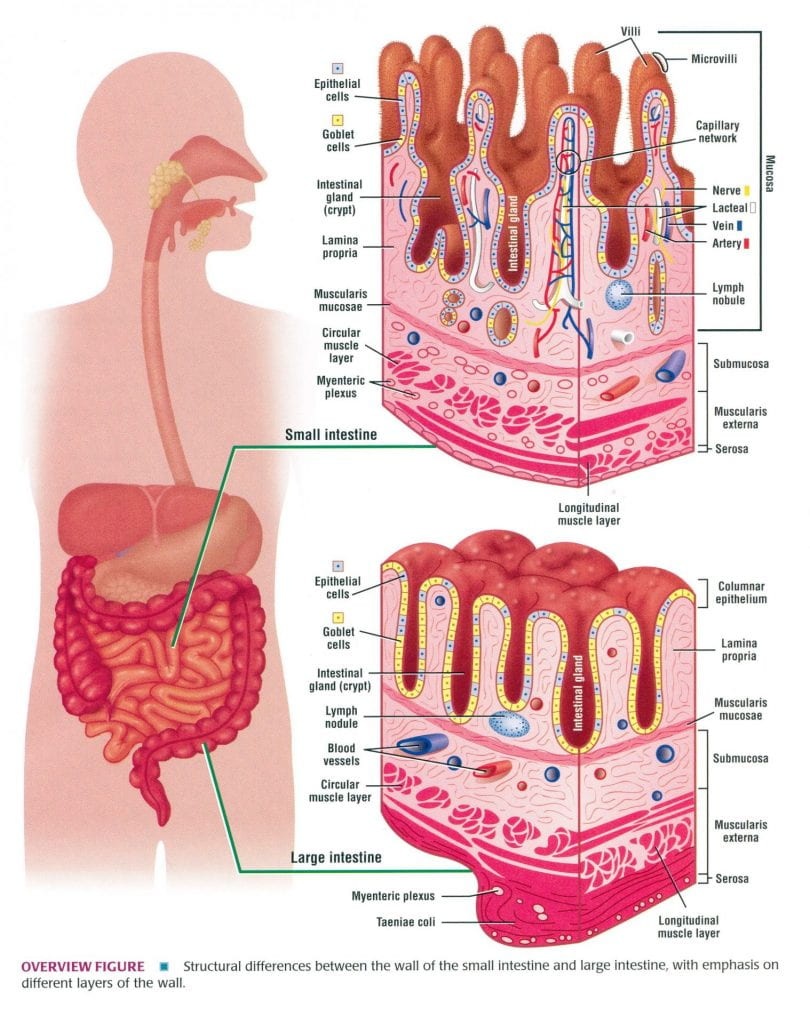
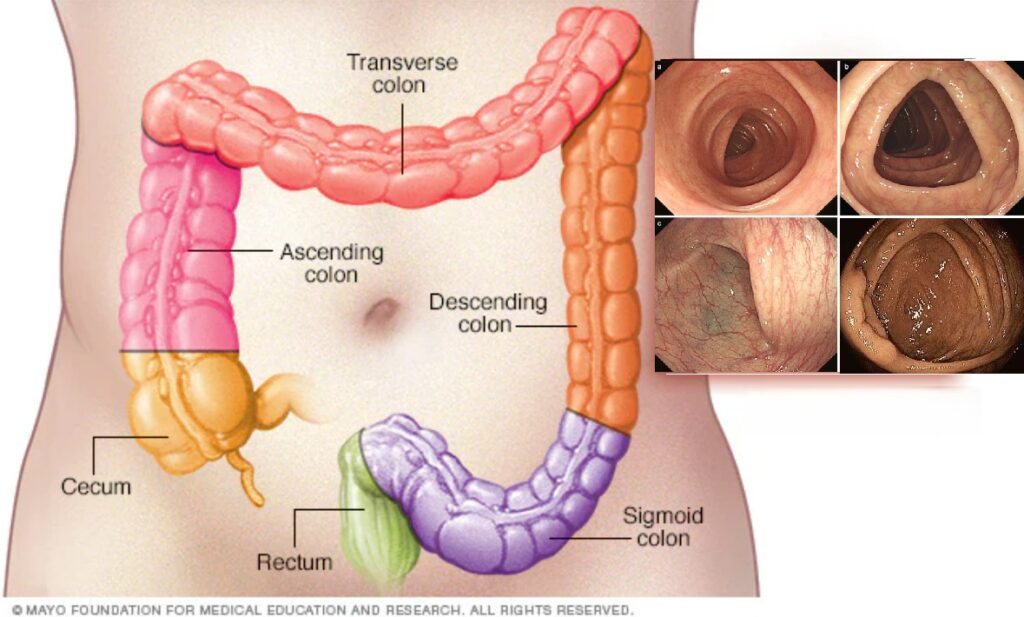
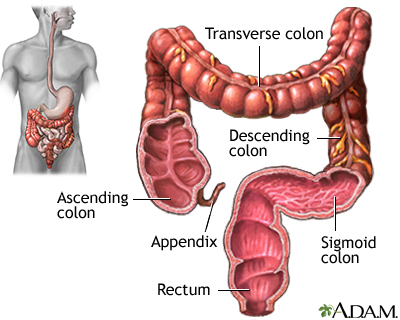
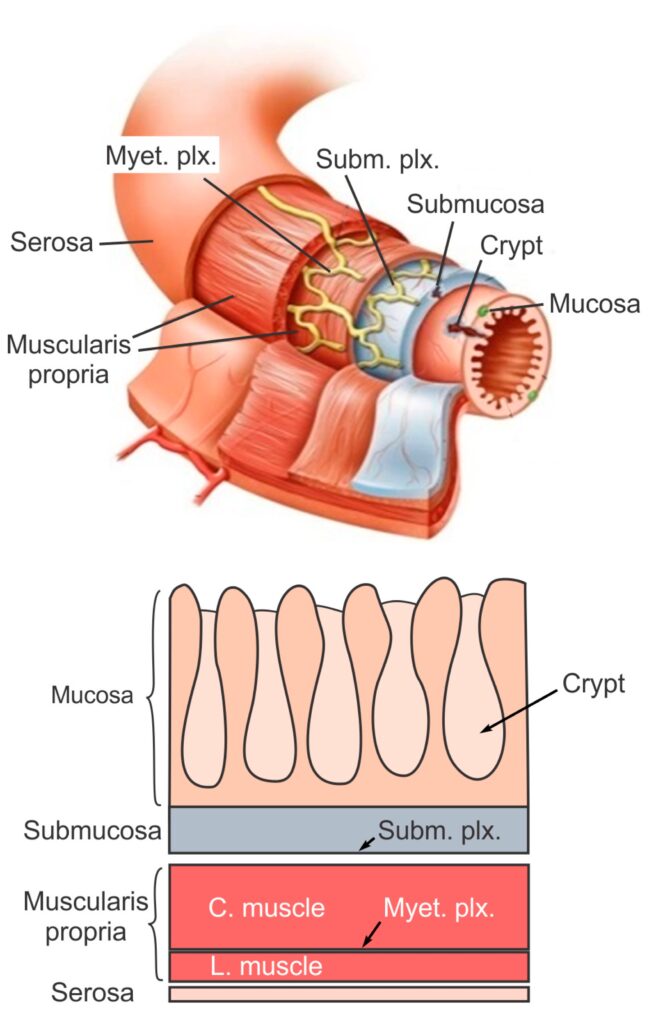
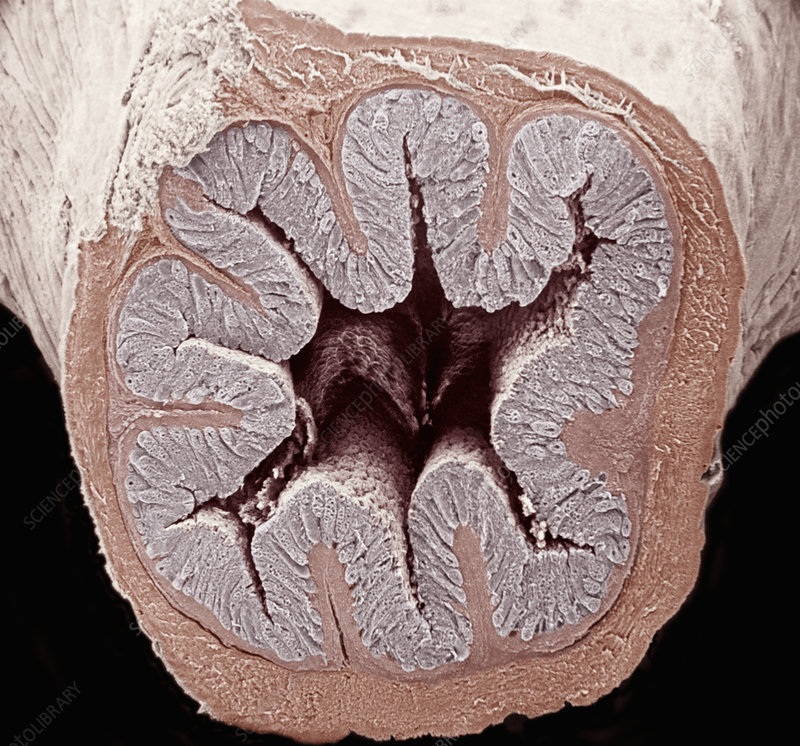
The small intestine (also known as the small bowel) is the longest portion of the digestive tract - it is more than 6 meters long and is located within the middle of the abdomen. It has three sections, the duodenum, jejunum and ileum. It completes the digestion of dietary fats, proteins and fats. The inner lining contains very small finger-like bumps called 'villi' which increase the surface available for absorption. The final nutrients produced are absorbed through this lining and transferred to the bloodstream. The large intestine (also known as the colon) reabsorbs water, nutrients and maintains the fluid balance of the body. It also processes undigested material (fibre) and stores waste before it is eliminated.
The large intestine (also known as the colon) reabsorbs water, nutrients and maintains the fluid balance of the body. It also processes undigested material (fibre) and stores waste before it is eliminated.
Dr Samuel treats these common bowel disorders :
- Coeliac disease
- Crohn’s Disease and Ulcerative colitis
- Iron deficiency
- Lactose intolerance
- Microscopic Colitis
- Colorectal Cancer - Sporadic and Hereditary
- Familial Adenomatous Polyposis (FAP) and Hereditary Nonpolyposis Colorectal Cancer (HNPCC)
- Irritable Bowel Syndrome (IBS) and other functional gut disorders
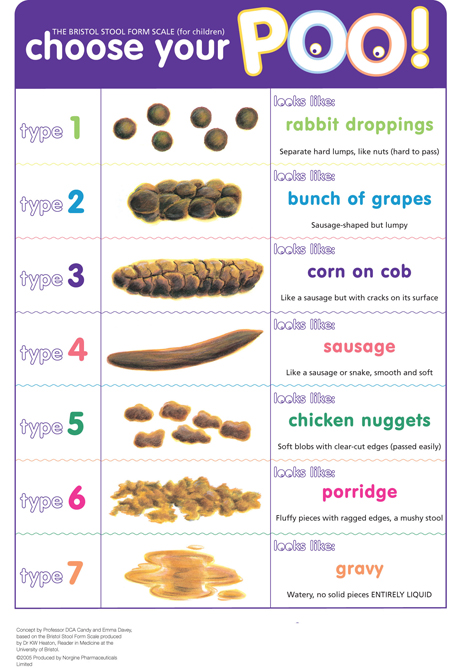
- Constipation
- Diarrhoea
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder (FGID) affecting one in seven Australian adults and is also common in the USA, Europe and many Asian countries. This condition is characterised by chronic and relapsing symptoms; lower abdominal pain and discomfort, bloating, wind, distension and altered bowel habit (ranging from diarrhoea to constipation) but with no abnormal pathology. The diagnosis of IBS/FGID should be made by a medical practitioner
- Pelvic floor dysfunction
The pelvic floor is a muscle sheet which closes the pelvis from below and above sit the bladder, uterus (womb) and rectum. The openings from these organs, the urethra from the bladder, the vagina from the uterus and the anus from the bowel pierce through the pelvic floor. Pelvic floor weakness can occur with a difficult childbirth or straining over time from constipation, heavy lifting, excess coughing or being overweight and can be worsened by hormonal changes at menopause, and with aging. Patients can develop downward slippage of organs causing rectal intussusception or prolapse. Conditions related include: faecal incontinence, obstructed defaecation syndrome, chronic anorectal pain, solitary rectal ulcer syndrome. Often patients improve with diet, stool softeners and pelvic floor retraining with biofeedback. Surgery may be needed.
- Faecal incontinence
- Haemorrhoids and anal fissure