Refractory coeliac disease - what to do when gluten free is not working
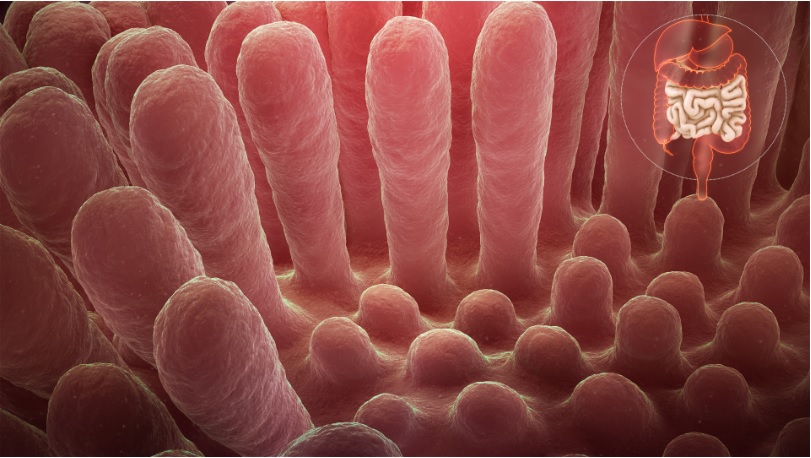
Coeliac disease is a systemic immune condition occurring in genetically susceptible individuals. An abnormal inflammatory response to dietary gluten in wheat, rye and barley results in damage to the small bowel mucosa and later villous atrophy with malabsorption. It is estimated that 1 in 70 Australians have coeliac disease and only 20% of those, have been formally diagnosed. In addition to gastrointestinal symptoms, the disease has extraintestinal manifestations, such as osteoporosis, dermatitis herpetiformis, neurological and psychological problems, liver disorders, arthritis and obstetric problems.
The only effective treatment for this lifelong disorder, at present, is a gluten-free diet (GFD) which is highly burdensome, requires long-term patient motivation, compliance and follow-up. In one study on the severity of health burden of various illnesses, the GFD was ranked second only to kidney failure with dialysis and above patients with diabetes on insulin, irritable bowel syndrome, inflammatory bowel disease, and heart failure:
"Prescribing a gluten-free diet should not be taken lightly. The diet is expensive, socially isolating and there is some evidence that questions the nutritional adequacy of a gluten-free diet when used in conditions other than coeliac disease. Given the false–positive rate with serology, commencing a strict life-long gluten-free diet is not recommended without a definite diagnosis of coeliac disease. A gastroscopy for small bowel (duodenal) biopsy is the gold standard and is recommended for all patients to confirm the diagnosis. It is generally a well-tolerated procedure with few risks." ...more information.
Some patients experience persistent symptoms due to inadvertent or deliberate gluten ingestion, a comorbid GI condition or refractory coeliac disease. Many adult patients fail to achieve complete histological healing of their small bowel mucosa despite adherence to a GFD. Several new treatments are under-development, including immunomodulators, biologics, vaccines and specific proteolytic enzymes. These should address the needs of patients with non-responsive coeliac disease with continuing symptoms and incomplete mucosal healing despite a GFD. They might also lighten the burden of a GFD in vulnerable patient groups, such as those with concomitant diabetes mellitus or neurodevelopmental/behavioural conditions. This page gives an approach when the gluten free diet seems not to be working.
What can I expect from my specialist if refractory coeliac disease is suspected?
Refractory CD is rare and existing definitions have problems. Treatments include immunomodulation with open-capsule budesonide, thiopurine and methotrexate. It is a subject of controversy whether asymptomatic patients may be labelled with refractory coeliac disease. There is not great evidence on the long term effects especially in patients that otherwise feel well. There are several steps to consider carefully:
- persistent or recurrent malabsorption symptoms (usually diarrhoea, weight loss)
- villous atrophy (Marsh III) on biopsy despite 6-12 months of gluten free diet supervised by expert coeliac dietitian
- confirm original coeliac disease diagnosis was correct
- Consider other causes of persistent symptoms (if coeliac disease diagnosis is confirmed)
- Consider other causes of villous atrophy (particularly if coeliac disease diagnosis is in doubt)
How common is non-responsive coeliac?
In recent years, endoscopy and biopsy studies have shown that non-responsive coeliac disease includes a larger group of patients than previously thought. While current scientific literature indicates that about 30 percent of patients have non-responsive coeliac disease, there is evidence the number is closer to 50 percent when those who don’t have symptoms but continue to have damage to the intestine, called mucosal atrophy, are included. The rate of persistent villous atrophy decreases with time on the GFD, so most individuals with celiac disease may eventually have mucosal recovery. Overall, only 1/3 of adults have normal villous architecture (a healthy, healed intestine on duodenal biopsies) after 2 years on a GFD and 2/3 after 5 years on a GFD.
Causes of non-responsive coeliac disease
| Gluten contamination (36-51%) |
| Microscopic colitis (colon biopsies) |
| Bacterial overgrowth (2 wk antibiotic trial) |
| Pancreatic insufficiency (faecal elastase, pancreatic enzyme trial) |
| Fructose/lactose/fructan/FODMAP intolerance or change in fibre |
| Irritable bowel syndrome or other functional gut disorder |
| Refractory coeliac disease (IHC, T cell clonal rearrangement by PCR) |
| Major Causes of Villous Atrophy in Adults
Pathologic findings characteristic but not diagnostic |
| Coeliac Disease ( review original histopathology sides with >2+4 biopsies, positive tTGA/EMA serology, positive HLA DQ2/6 genotyping, biopsy-proven dermatitis herpetiformis, siblings with coeliac disease, and prior response (symptoms +/- histology) to and years on GFD) |
| Tropical Sprue (check travel history: India and South East Asia, Centra/South America, West Africa; folate deficiency, TI villous blunting, folate 5mg daily + tetracycline 250mg qid 3/12 with response by 2 weeks) |
| Adult-onset autoimmune enteropathy (60% male, anti-enterocyte or anti-goblet cell) |
| Hypogammaglobulinemia (exclude CVID) |
| Idiopathic AIDS enteropathy |
| Pathologic findings could be diagnostic |
| Eosinophilic gastroenteritis |
| Whipple disease |
| Abetalipoproteinemia |
| Intestinal lymphoma |
| Collagenous sprue |
| Tuberculosis |
| Giardiasis |
| Crohn’s disease |
| Pathologic findings are non-specific |
| Small-bowel bacterial overgrowth (trial 2wks metronidazole 400mg tds) |
| Infectious enteritis and parasitic infestation |
| drug-induced enteropathy (eg. sartans/NSAIDs/statins) |
|
Severe malnutrition |
| Small-bowel ischemia |
Could there still be gluten in my diet?
Individual coeliac disease responses to gluten exposure are highly variable, but a chronic gluten exposure of at least 50 mg for more than a month will likely induce intestinal damage. One British gluten exposure study suggested that over a 6 month period 1/3 had intentional exposure, 1/3 had unintentional exposure and 1/3 felt they were strictly gluten free. Depending on the centre, 36-51 percent of patients with non-responsive coeliac disease are inadvertently consuming gluten.
You'll need a repeat biopsy after 6 months of a strict gluten free diet. Particularly if you have low titre tTG IgA, you'll need an expert coeliac dietitian.
- Ensure you are not consuming wheat which can be labeled as as bulgar, farina, food starch, kamut, semolina, spelt, triticale, durum.
- Recheck you are not consuming hidden gluten, ubiquitous in: toothpaste, glues, play-do, envelope or postage stamp gum, cosmetics such as lipstick and lip balms, medications and vitamins and supplements, naturally "safe" GF grains (soy, millet, buckwheat, rice and sorghum flour may have gluten-containing grains introduced during planting, harvesting, or processing), soya sauce and other sauces, fried foods, seasonings, processed meats including hot dogs and meat patties, food additives, ice cream, and even in rice cakes.
- Recheck labels of favourite everyday foods, as ingredients can change without notice
- Contact manufacturers of products that contain the statement “manufactured in a plant that also produces or used on a machine that also processes wheat” to ask about the procedures they use to avoid cross-contamination
- Recheck all over-the-counter and prescription medications with the manufacturers to be sure they do not contain gluten
- Evaluate religious ceremony/holiday foods or communion hosts to be sure they contain less than 20 parts per million of gluten
- Evaluate frequency and strategies used when dining away from home. Food preparation details matter: dusting meat with flour before grilling, using stock to cook rice, or steaming vegetables in the pasta water is not disclosed on menus.
- Ensure any ingested oats are certified gluten free and evaluate the tolerance of gluten-free oats in the diet. The addition of uncontaminated oats to the GFD has been tolerated by the majority of CD patients; however, a few people with CD may be clinically intolerant to oats
- Look for sources of cross-contamination at home, and ensure the following are implemented in the home: Use a separate toaster; Thoroughly clean kitchen counters; Use clean or separate cooking and serving utensils; Avoid “double dipping” in common condiment jars.
