Hepatitis C treatment
There has been a major leap forward in the management and treatment of hepatitis C. A new generation of medications are now available which are more effective, easier to take and have fewer side-effects than the older medications. The Australian Government has listed some of these on the Pharmaceutical Benefits Scheme (PBS). Over the months and years, it is likely they will add more. Australia is now a world leader in publicly-funded access to these new, highly effective medicines.
What are the new medicines?
The new, direct-acting antiviral (DAA) medicines available on the PBS since Augst 2018 are:
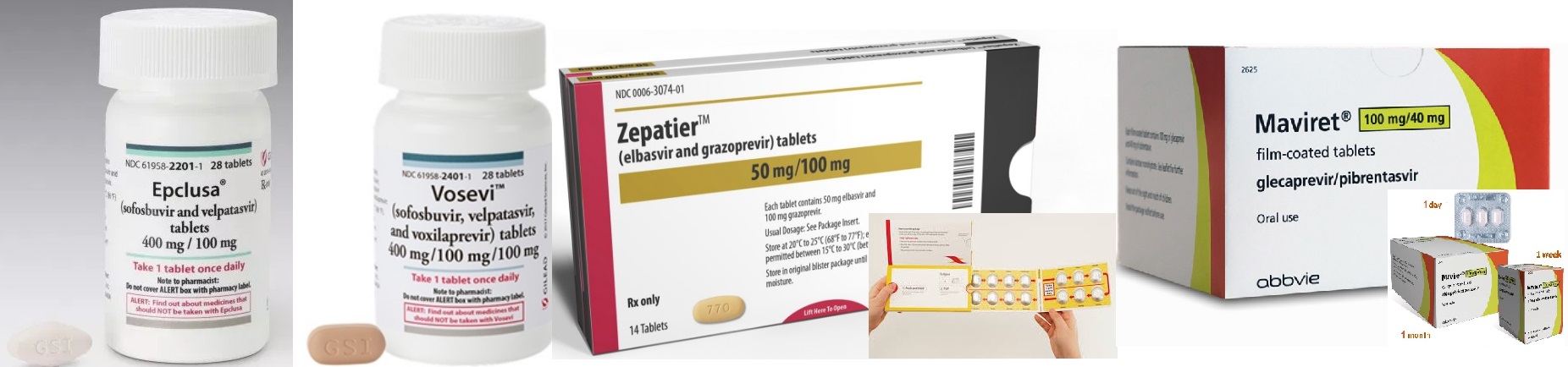


- sofosbuvir + velpatasvir (Epclusa®)
- sofosbuvir + velpatasvir + voxilaprevir (Vosevi®)
- elbasvir + graoprevir (Zepatier ®)
- glecaprevir + pibrentasvir (Maviret ®)
- ribavirin (Ibavyr®)
Are the new medicines better than the previous ones?
Yes, the new DAA medicines are:
- more effective, resulting in a cure for 90-95% of people
- taken as tablets only and have very few side-effects
- taken for as little as 8-12 weeks in most cases, and
- provide interferon-free treatment options for all common genotypes in Australia.
Are the new medicines available for all people with Hepatitis C?
Yes, treatment using the new DAA medicines is available through the PBS for all people living with hepatitis C over the age of 18 and who have a Medicare Card. The specific combination of medicines used depends on genotype, prior treatment experience and whether there is cirrhosis (liver scarring), among others.
Are there interferon-free options available for all genotypes?
Interferon-free treatment options are available for genotypes 1-6
What information will the doctor need to know about your health before treatment can be prescribed?
There are a number of tests the doctor will do and information you will be asked to provide before treatment can be prescribed. These include:
- blood tests to confirm you have active hepatitis C infection
- blood tests to determine the hepatitis C genotype (strain) you have
- assessing to see if you have developed cirrhosis (liver scarring)
- discussing any previous treatments for hepatitis C you may have taken,
- identifying any other illnesses or health complaints you have, and
- discussing any other prescription medications, over-the-counter medications or substances you are taking, to avoid any possible drug interactions.
- discussing readiness to start treatment and discuss things that may impact on your ability to take the medicine regularly, as prescribed
What does treatment with the new medicines involve?
The treatment regimens for the new DAA medicines range between 8 and 24 weeks for a complete course of treatment, depending on your genotype, treatment history, whether you have cirrhosis and the combination of medicines used. Some treatments require only 1 to 2 tablets once or twice a day. For others, up to three medicines may be required or an injection (peg-interferon) may be used together with tablets.
What monitoring will I need during treatment?
If you do not have cirrhosis, then Dr Samuel and his nurse will usually do this at the start (DS rooms), at week 2 (nurse call), week 4 (DS rooms), week 8 (nurse call), at end of treatment (DS rooms) and then at 12 weeks after the end of treatment (nurse call) with final review 16 weeks (DS rooms). For a routine 12 week course, you will need bloods at the start (FBC, UEC, LFT, INR, HCV RNA level), week 4 (FBC, LFT +/- HCV PCR qual), week 12 (FBC, LFT, HCV PCR qual), and week 24 (FBC, LFT, HCV PCR qual). If you have cirrhosis and if you are on ribavirin, then Dr Samuel and his nurse will usually monitor you and your liver function more closely; usually checking in every 2 to 4 weeks with bloods at week 2, week 4 and then every 4 weeks while on treatment.
Can General Practitioners (GPs) prescribe treatment for hepatitis C?
Yes. Before prescribing any medicines, your GP will be required to collect information and conduct tests (see above) to establish which combination of medicines will be the most effective for you. Based on that information, the GP will then consult with a specialist before prescribing the medicine for you. You will probably need a couple of appointments before receiving a prescription. In some cases, your GP may refer you to Dr Samuel or another specialist before treatment is commenced.
Can you still see your specialist to access the new medicines?
Yes, gastroenterologists, hepatologists or infectious diseases physicians experienced in the treatment of chronic hepatitis C will continue to prescribe the new medicines. These specialists will also provide advice to GPs prescribing the new medicines, so you may consider seeing your GP if this is more convenient for you.
Where can you get your prescription filled?
Most prescription can usually be filled by your local pharmacy. However, due to the very high cost of the medicines, some are experiencing a few days delay. This situation should improve over time as more people start accessing treatment. Some prescriptions may only allow you to collect 4 weeks’ supply of medicine at a time. So it is important to plan ahead so you don’t run out of medicine.
How much do the medicines cost you?
You will be charged the usual co-payment price ($38.30 for general patients and $6.20 for concessions). The doctor can only prescribe one medicine per "authority" prescription, so you may be required to pay the dispensing fee for each medicine.
Do I need to take extra precautions on treatment?
Both men and women need to use reliable contraceptives to avoid falling pregnant during and for ribavirin up to 6 months after hepatitis C treatment. Otherwise, the precautions are the same for anyone with hepatitis C. Household and sexual transmission is extremely unlikely. However, as hepatitis is transmitted through direct blood to blood contact, even if small, do not share toothbrushes, nail clippers and razors and clean up blood spills at home. You can't donate blood. Hepatitis C (unlike hepatitis B and HIV) is not considered a sexually transmissible infection, as it is not present in sexual fluids in quantities large enough to allow transmission. Sexual transmission is very rare (0-0.06%/year) among long term monogamous partners. Caution should be exercised where skin trauma can occur including anal intercourse, rough sex, the use of sex toys or where a partner has a condition causing skin irritation in the genital area. Ask your doctor about further protecting your liver with hepatitis A and B vaccination. You are at risk of faster progression to liver disease, if you drink more than 4 standard alcohol drinks a day and so talk with your doctor about stopping completely. There is no evidence that herbs including Milk thistle improves hepatitis C outcome. Your doctor will discuss with you any drug-drug interactions which might occur with the DAAs.
Are the side effects or drug interactions?
Most have no side effects or drug interactions. Less than 15% on new DAAs suffer mild to moderate rash, fatigue, headache, nausea, diarrhoea or insomnia. Talk to your doctor about potential drug and herb interactions as fine tuning may be required. With Harvoni special precautions are needed with stomach acid reducing agents (antacids, ranitidine, omeprazole), heart antiarrhythmics (digoxin, amiodarone), anticonvulsants (phenytoin, carbemazepine), herbal supplements (St John's wort) and the cholesterol treatment, rosuvastatin. Daklinza may interact with dabigatran, statins, clarithromycin and ketoconazole. Ribavirin can cause anaemia. If you are over 65 years, then you may present extra challenges as you may progress more rapidly to cirrhosis, are more likely to suffer from fatigue and to require changing medications to avoid drug interactions.
What if treatment is not effective for you?
For most people it is highly likely the new DAA medicine will be effective. If the new treatment does not work for you, your doctor will refer you for further assessment .
What is the risk of no treatment?
Most living with hepatitis C have no symptoms. Some experience fatigue, nausea or abdominal discomfort. Chronic hepatitis C is a slowly progressive viral infection, with approximately 5–7% progressing to cirrhosis (liver scarring) by 20 years. Some progress faster including those with significant alcohol ingestion (>40 g/day), co-infection with hepatitis B or HIV, age over 40 years at acquisition, coexistent liver diseases (eg. nonalcoholic steatohepatitis NASH), marijuana use, diabetes and obesity. Women appear to progress more slowly than men. Cirrhosis moves through different stages each with higher risks of life threatening bleeding, liver cancer, encephalopathy ("brain fog"), fluid overloading and bacterial infections.
Where can you get further information?
You can talk to your GP, specialist, Dr Samuel's specialist hepatitis C nurse or call the National Hepatitis Information line on 1800 437 222.
